Blog
New research reveals why clinicians bypass your carefully designed protocols—and what you can do about it
Your healthcare organization has invested millions in developing comprehensive order sets, yet clinicians continue scrambling to place additional orders within minutes of using these protocols. Our new study reveals exactly why this disconnect is costing the industry billions.

New research reveals why clinicians bypass your carefully designed protocols—and what you can do about it
The $5,000-Per-Provider Problem
Phrase Health's analysis of over 65 hospitals uncovered a startling reality: providers consistently supplement order sets with additional orders. This translates to over 5,000 additional orders annually per experienced provider, representing 15 hours of lost productivity and $3,000-$5,000 in wasted labor costs per provider.
Experienced residents order outside of order sets at nearly twice the rate of their peers—a 240% increase signaling fundamental workflow limitations.
Four Critical Patterns of Order Set Failure
"Great catch—let's just add it" - Missing orders that should be included, like prednisone consistently added after pulmonary discharge sets.
"Wait… why are we doing that?" - Clinicians add orders purposely excluded due to contraindications. This requires targeted education and "do-not-order" guidance.
"I know it's in there somewhere" - Orders buried within complex sets. This UI friction can be addressed by streamlining layouts.
"This patient had other conditions" - Appropriate additional orders for patient-specific needs outside the order set's scope.
The 25% problem: orders hidden in plain sight
The most striking finding: approximately 25% of orders placed within five minutes actually existed in the original order set but were overlooked by busy clinicians. This highlights critical usability issues addressable through better design.
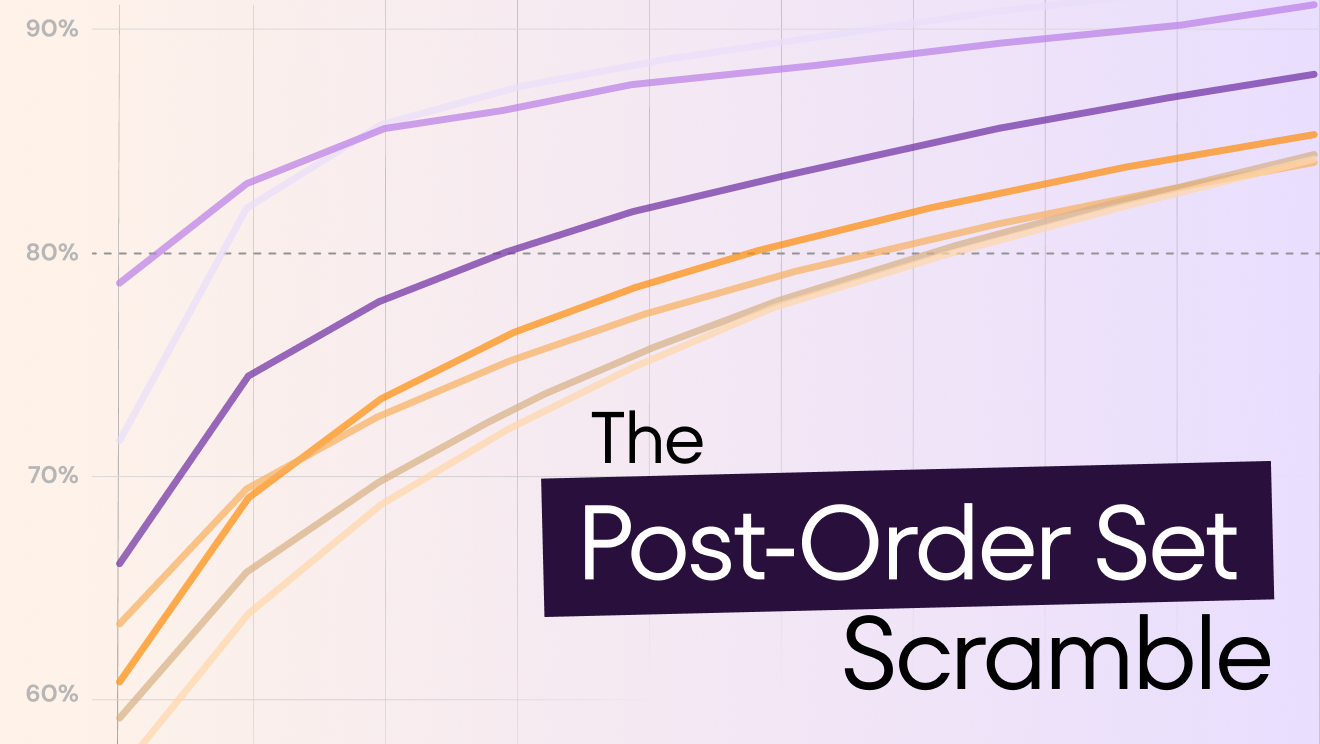
Where the biggest opportunities lie
Medications: Cardiovascular drugs showed high variation rates (153%), likely due to chronic medications difficult to standardize. Antineoplastics had the highest follow-up rates (246%) but lowest overall volumes.
Non-medication orders: Imaging requests (39%) and referrals/consults (34%) drove most additional ordering activity. Given imaging's impact on length of stay, these findings warrant enhanced decision support.
The provider type divide
Providers who can authorize orders—attendings, residents, fellows, and APPs—consistently showed 16-18% supplemental ordering rates. Support staff who only queue orders showed significantly lower rates of 2-6%, suggesting that decision-makers identify patient needs that don't fit standardized workflows.
The hidden costs of poor governance
Basic governance processes for 600 order sets cost approximately $750,000 in staff time, while robust review of half the library exceeds $2 million in personnel costs. These figures don't account for downstream costs and patient safety implications.
Moving beyond "work as imagined"
The fundamental challenge lies in the gap between "work as imagined" and "work as done." Order sets designed in conference rooms may satisfy guidelines but fail to meet practical bedside needs.
The orders within five minutes metric helps healthcare systems identify which deviations represent design gaps versus appropriate clinical judgment, providing more targeted optimization strategies than traditional governance approaches.
Ready to uncover hidden inefficiencies in your order sets? The full Post-Order Set Scramble report provides detailed benchmarking data, implementation frameworks, and actionable optimization strategies.
Your healthcare organization has invested millions in developing comprehensive order sets, yet clinicians continue scrambling to place additional orders within minutes of using these protocols. Our new study reveals exactly why this disconnect is costing the industry billions.

Written by
The Phrase Team
Sep 10, 2025
Written by
The Phrase Team
Sep 10, 2025
The $5,000-Per-Provider Problem
Phrase Health's analysis of over 65 hospitals uncovered a startling reality: providers consistently supplement order sets with additional orders. This translates to over 5,000 additional orders annually per experienced provider, representing 15 hours of lost productivity and $3,000-$5,000 in wasted labor costs per provider.
Experienced residents order outside of order sets at nearly twice the rate of their peers—a 240% increase signaling fundamental workflow limitations.
Four Critical Patterns of Order Set Failure
"Great catch—let's just add it" - Missing orders that should be included, like prednisone consistently added after pulmonary discharge sets.
"Wait… why are we doing that?" - Clinicians add orders purposely excluded due to contraindications. This requires targeted education and "do-not-order" guidance.
"I know it's in there somewhere" - Orders buried within complex sets. This UI friction can be addressed by streamlining layouts.
"This patient had other conditions" - Appropriate additional orders for patient-specific needs outside the order set's scope.
The 25% problem: orders hidden in plain sight
The most striking finding: approximately 25% of orders placed within five minutes actually existed in the original order set but were overlooked by busy clinicians. This highlights critical usability issues addressable through better design.
Where the biggest opportunities lie
Medications: Cardiovascular drugs showed high variation rates (153%), likely due to chronic medications difficult to standardize. Antineoplastics had the highest follow-up rates (246%) but lowest overall volumes.
Non-medication orders: Imaging requests (39%) and referrals/consults (34%) drove most additional ordering activity. Given imaging's impact on length of stay, these findings warrant enhanced decision support.
The provider type divide
Providers who can authorize orders—attendings, residents, fellows, and APPs—consistently showed 16-18% supplemental ordering rates. Support staff who only queue orders showed significantly lower rates of 2-6%, suggesting that decision-makers identify patient needs that don't fit standardized workflows.
The hidden costs of poor governance
Basic governance processes for 600 order sets cost approximately $750,000 in staff time, while robust review of half the library exceeds $2 million in personnel costs. These figures don't account for downstream costs and patient safety implications.
Moving beyond "work as imagined"
The fundamental challenge lies in the gap between "work as imagined" and "work as done." Order sets designed in conference rooms may satisfy guidelines but fail to meet practical bedside needs.
The orders within five minutes metric helps healthcare systems identify which deviations represent design gaps versus appropriate clinical judgment, providing more targeted optimization strategies than traditional governance approaches.
Ready to uncover hidden inefficiencies in your order sets? The full Post-Order Set Scramble report provides detailed benchmarking data, implementation frameworks, and actionable optimization strategies.

.svg)
.svg)